Coley’s Cancer-Killing Concoction
 A macrophage (purple) attacks a cancer cell (yellow)On October 1st 1890, William B. Coley, a young bone surgeon barely two years out of medical school, saw one of his first patients in private practice at the New York Memorial Hospital. Although he’d only finished his residency earlier the same year, he'd already gained a good reputation and many considered him a rising star of the New York surgical scene.
A macrophage (purple) attacks a cancer cell (yellow)On October 1st 1890, William B. Coley, a young bone surgeon barely two years out of medical school, saw one of his first patients in private practice at the New York Memorial Hospital. Although he’d only finished his residency earlier the same year, he'd already gained a good reputation and many considered him a rising star of the New York surgical scene.
The seventeen year old patient had a painful, rapidly growing lump on the back of her right hand. She had pinched the unlucky appendage between two railway carriage seats on a transcontinental trip to Alaska some months before, and when the bruise failed to heal she assumed the injury had become infected. However the bruise turned into a bulge, the pain steadily worsened, and her baffled doctors were eventually compelled to call for Dr. Coley. As a surgical man, Coley would never have guessed that this innocuous referral would take his career in a totally new direction– into an unusual branch of medicine now known as cancer immunotherapy.
At first Dr. Coley was also uncertain about the diagnosis. But as the girl’s condition rapidly deteriorated– with the lump becoming larger, more painful, and associated with the loss of sensation in some of the surrounding skin– the awful truth became apparent. She had a sarcoma, a type of cancer that affects bone and connective tissue in the body. Unfortunately, 19th century medicine offered very few treatment options.
On November 8th, Coley amputated her arm at the elbow. Although the operation appeared to go well, the girl– named Elizabeth Dashiell– developed severe abdominal pain three weeks later. Soon thereafter she noticed more lumps in her breasts and armpits, signs that the cancer was metastasizing, or spreading. She rapidly lost strength and died on January 23rd 1891, a scant three and a half months after her initial consultation, with a traumatized Dr. Coley at her bedside.
Elizabeth’s death hit the young surgeon hard. While a more experienced physician might have shrugged away the apparent failure and moved on, Coley was determined to do something. His ensuing efforts culminated in the development of a famous fluid that, for a time, appeared to promise the fulfillment of that long-held dream: a universal cure for cancer.
Coley began by poring through the hospital’s records, looking for clues from previous sarcoma cases that might lead to better treatments in the future. He soon found what he was looking for: the case of a German man who came to the hospital with an egg-sized sarcoma in his left cheek some seven years earlier. There were several attempts to excise the tumour but none of them were successful– each time the cancer came back, as aggressive as before. The final operation could only partially remove the huge mass, leaving an open wound that subsequently became infected.  William B. ColeyThe unfortunate immigrant was deemed a terminal case.
William B. ColeyThe unfortunate immigrant was deemed a terminal case.
Yet four and a half months later, the man was discharged with no trace of disease. Coley personally tracked down the former patient to verify that the miraculous cure had taken place. Indeed, the man was healthy and happily settled into his new life in the United States. The records showed that after the wound became infected with a commonplace bacterium, Streptococcus pyogenes, the patient went through several bouts of fever. With each attack of fever the tumour shrank until eventually it disappeared entirely, leaving only a large scar under the left ear. Coley surmised that the infection had stimulated the German’s immune system– as evidenced by the repeated fevers– and that it was this immune response that had caused the eradication of the cancer.
The story so convinced Coley that he– perhaps cavalierly– contrived to contaminate his next ten suitable sarcoma cases with Streptococcus. His initial approach was to inject a solution of live bacteria deep into the tumour mass on a repeated basis over several months. The first patient to undergo this treatment was a bedridden man with inoperable sarcoma in the abdominal wall, bladder, and pelvis. Using this experimental method, the patient was cured spectacularly. He staged a full recovery, and survived another twenty-six years before dying from a heart attack. But subsequent results were mixed; sometimes it was difficult to get the infection to take hold, and in two cases the cancer responded well to treatment but the patients died from the Streptococcus infection.
Coley’s discovery, as it turns out, was actually a re-discovery. The idea of a link between acute infection and the resolution of tumours was not new, and the phenomenon of infection-related "spontaneous regression" of cancer has been documented throughout history. A 13th century Italian saint was reputed to have his tumour-afflicted leg miraculously healed shortly after the malignant growth burst through the skin and became infected. Crude cancer immunotherapies working along similar lines to Coley’s early experiments were known in the 18th and 19th centuries, and may extend back to the time of the pharaohs. Ancient writings suggest that the renowned Egyptian physician Imhotep may have used a similar infect-and-incise method to treat tumours.
But Coley took those first important steps in dragging this old remedy into the twentieth century. After the fatalities with the ‘live’ version of his therapy, he developed an improved fluid containing killed bacteria of two different strains, Streptococcus pyogenes and Serratia marcescens. This was based on the idea that the dead bacteria would still have the immune-stimulating capability of their living brethren (in the form of purported ‘toxins’), but not share their inconvenient tendency to cause death.  Streptococcus pyogenesHis invention became variously known as ‘Coley’s Toxins’, ‘Coley’s Vaccine’, ‘Mixed Bacterial Toxins’ or ‘Coley Fluid.’ The treatment was met with considerable success, with one study in 1999 suggesting that it was at least equally as effective in treating cancer as conventional modern therapies. With due care in dosing and management of the induced fever, it was also remarkably safe.
Streptococcus pyogenesHis invention became variously known as ‘Coley’s Toxins’, ‘Coley’s Vaccine’, ‘Mixed Bacterial Toxins’ or ‘Coley Fluid.’ The treatment was met with considerable success, with one study in 1999 suggesting that it was at least equally as effective in treating cancer as conventional modern therapies. With due care in dosing and management of the induced fever, it was also remarkably safe.
Although Coley took the concept of immunotherapy much further than his pharaonic forebears, he had no clear idea how his toxins actually worked, and the tools did not yet exist for him to find out. But given the rapid scientific progress at the turn of the last century, he reasoned that a deeper understanding of his therapy would arrive soon enough. Although the true extent of his "Toxin" success has been questioned by historians, the validity of his approach has never been seriously called into doubt. Indeed his results are regularly cited in the cancer research literature to this day.
Over the following years Coley continued to refine his technique. He determined that the toxins should be administered to patients at progressively higher doses to counter the body’s innate "immune tolerance" to the treatment. Other physicians in America and Europe also experimented with the method, and found that the toxins appeared to work just as well in a number of different non-sarcoma cancer types such as carcinoma, lymphoma, and melanoma. They could also be given intravenously some distance from the site of the tumour, and still be effective. Variations on the basic bacterial recipe and different dosing regimes were tried, depending on the individual patient and the particular cancer’s type and proliferation. Through his career Coley himself treated over one hundred patients with his concoction, and countless more were treated by other doctors.
As the fame of his fluid grew, so did Dr Coley’s stature: in 1915 he became head of the Bone Service at the New York Memorial Hospital (which later became the Memorial Sloan-Kettering Cancer Center). By the time he died in 1936, Coley’s Toxins were mentioned in a number of different surgical textbooks as a standard anti-cancer therapy.
Conventional modern medicine, however, very rarely employs Coley’s Toxins in the treatment of cancer, for reasons almost as complicated as the human immune system itself. One concern is the far-from-complete understanding of the mechanism of action; generally, doctors are reluctant to administer treatments whose workings they don’t fully comprehend. The stimulated human immune system is a whirling tempest of different physiological and biochemical responses, and even now there’s much uncertainty about how Coley’s Toxins modified this complex mechanism to better attack its cancerous target. 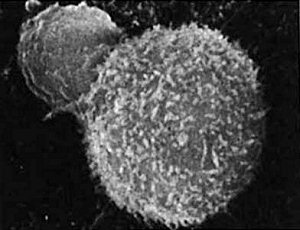 T-cell (small sphere) attacks a cancer cellOne theory stresses the importance of the fluid-induced fever in killing the cancer cells; another considers the debris-engulfing macrophage cells to be the main players, while others consider various different immune messenger molecules– or cytokines– to be important.
T-cell (small sphere) attacks a cancer cellOne theory stresses the importance of the fluid-induced fever in killing the cancer cells; another considers the debris-engulfing macrophage cells to be the main players, while others consider various different immune messenger molecules– or cytokines– to be important.
The eclipsing of Coley’s Toxins also had something to do with the concurrent development of radiation therapy and, a little later, chemotherapy. Soon after Wilhelm Roentgen discovered X-rays in 1895, the possibility of using radioactivity to treat cancer was investigated. The technology was exciting, new, and developing fast along well-understood principles. Although the first results of radiotherapy weren’t all that impressive, it had the advantage of fractional doses, and once the equipment was in place it didn’t require the complicated, patient-specific preparation which was needed with Coley’s Toxins. Likewise chemotherapy was based on known scientific principles, and could be manufactured and used relatively easily.
Furthermore, both radiotherapy and chemotherapy have an immune-suppressing side-effect. Since both treatments kill the rapidly dividing cells of the immune system along with the rapidly dividing cancer cells, both can be used together if care is taken. But immune-stimulating Coley’s Toxins work entirely differently, and their effect would be cancelled out if used at the same time as high-dose immunosuppressant chemo- or radiotherapy. It became an either/or situation– and in the end, the fashionable new treatments won out over Coley’s fiddly reworking of an ancient 'natural' remedy.
So when the US Food and Drug Administration changed the status of Coley’s Toxins to that of a 'new drug' in 1963– meaning that it could only be used in clinical trials, and greatly reducing its availability– it seemed that its time had already long passed. But cancer immunotherapy does have limited applications today. Perhaps its most frequent mainstream use is in the treatment of bladder cancer; solutions containing the tuberculosis vaccine are routinely instilled into cancer-affected bladders, and are effective in causing regression of tumour deposits. It is theorized that the bladder's immune response deals with the cancer in a similar way to the whole-body immune effect of Coley’s Toxins. 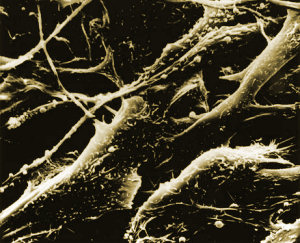 Melanoma cellsMelanoma, a particularly nasty type of skin cancer that responds poorly to conventional radiotherapy and chemotherapy, is sometimes treated with an immune-stimulating cytokine called interferon.
Melanoma cellsMelanoma, a particularly nasty type of skin cancer that responds poorly to conventional radiotherapy and chemotherapy, is sometimes treated with an immune-stimulating cytokine called interferon.
In some ways this century-old form of treatment is still a fringe area of medicine. But researchers have once again begun to probe the possibilities of immunotherapy. New antibody-based treatments like Mabthera and Herceptin are making a real difference in the treatment of common cancers like lymphoma and breast cancer. Although these therapies don’t stimulate the body’s immunity as a whole, they are based on antibody molecules which are key components of the human immune system. They show that our increasing knowledge of the molecular nitty-gritty of the body’s own defence and repair network is starting to make a real difference in the battle against cancer. One tumour at a time, such advances in modern medicine are finally vindicating William Coley and his one-hundred-year-old cancer-killing concoction.
Further reading:
Dr William Coley and tumour regression: a place in history or in the future
Cancer Research Institute, founded by Coley's descendants
Wikipedia: Dr. Willian B. Coley
Wikipedia: Coley's Toxins
Related Articles:
Unintentional, Unwitting Heroine
Non-Surgical Surgical Strikes
Poland's Biological Defensive
Cancer Assassins
Link is here!

Comments